Introduction: A number of endocrine abnormalities have been reported in people infected with HIV. Among these, hypogonadism is well described, particularly as men progress to AIDS and in those who are wasting. Testosterone has both anabolic and androgenic effects. Although there has been a study showing improvement in quality of life in HIV-positive men treated with high doses of Testosterone, there is no data confirming its usefulness as an anabolic agent. The recommendation is that Testosterone should not be used unless hypogonadism is proven.
Diagnosis: Although some patients present with classical signs and symptoms of androgen deficiency, many have less specific complaints. Symptoms may be particularly difficult to notice in patients with AIDS. Complaints may include decreased libido, erectile function, fatigue, depression, decreased frequency of shaving, and decreased bone density. Laboratory tests should include a total and free (or bioavailable) testosterone, FSH and LH.
Intramuscular Testosterone: Oral administration of testosterone is not practical and is generally not available in the US. The most commonly used testosterone replacement is intramuscular depot injections. This route has the advantages of ensuring delivery to the patient without concerns of patches slipping off or doses being forgotten. The drug itself is inexpensive. A significant problem is the rapid serum peak to supraphysiologic levels, reached between hours to a few days after injection of testosterone enanthate, then a gradual decline over the following weeks. There is no circadian variation in delivery.
Optimal dosing appears to be 200 mg IM testosterone enanthate every two weeks. Injections can be painful, especially in wasted patients, and usually require an office visit. Additional side effects, common to all forms of androgen replacement, may include acne and gynecomastia. Salt retention may be a problem in patients with preexisting congestive heart failure, cirrhosis or nephrosis.Testoderm scrotal patch: The TestodermR Testosterone Transdermal System is placed on clean, dry scrotal skin. The dosage is a 6 mg patch which is applied at 9 a.m. and worn for 22 to 24 hours each day. The scrotal hair must be dry-shaved for optimal contact; chemical depilatories should not be used. Men may be required to change to close-fitting underwear, and exercise and hot weather may cause the patch to come off. Follow-up bloods for total testosterone should be obtained 2-4 hours after patch placement 4-6 weeks after continuous therapy. If adequate levels are not reached by the end of 2 months, another form of therapy may be required.
In long term studies of hypogonadal HIV negative men, 60% maintained normal serum testosterone levels. Serum dihydrotestosterone (DHT) levels were elevated in all patients who had increases in serum testosterone levels.The significance of the increased DHT is unknown. Self report of mood, energy level and frequency of sexual thoughts and intercourse all increased over baseline, with nearly 50% of the patients reporting increases by week three.The most common side effect was local skin problems.
Androderm nonscrotal patches: Androderm R is a permeation-enhanced testosterone transdermal system that is applied to nonscrotal skin. Again, all studies were conducted on HIV negative, hypogonadal men, with no published literature on the use of Androderm in HIV positive subjects. Dosage is two patches, applied nightly in a rotating manner on the back, abdomen, upper arm or thigh.
In three clinical trials of 121 hypogonadal men, 92% of subjects achieved normal morning testosterone levels and 88% bioavailable testosterone. Pharmacokinetic studies show a steady testosterone level in a pattern mimicking the normal circadian.
Self-reported symptoms of impotence, decreased libido, fatigue, hot flashes and depression all improved. No changes were noted in aggression or hostility. In previously nonvirilized subjects treatment led to virilization and increases in lean body mass.
The most common adverse event was local skin irritation. In long term follow-up, 53% noted some form of local reaction at the application site. Of 121 men treated, 12 patients (9.8%) discontinued therapy due to a site reaction. Pruritus is the most common reaction reported (37%), followed by local blister formation (12%) or erythema (7%).
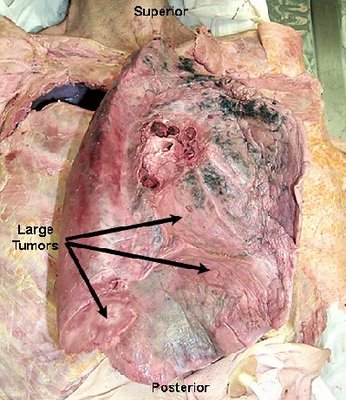
Contraindications to testosterone therapy: Androgen replacement is contra-indicated in men with known or suspected breast cancer, prostate cancer or Kaposi sarcoma. Fertility will decrease during testosterone treatment. Decreases in serum HDL, gynecomastia, and increases in prostate size are similar in all forms of TRT and generally not clinically significant.
Future research: Studies are now ongoing to evaluate the benefits of Testosterone on body composition in men with wasting (contact JC at 410-955-1373 or 955-9862). Previous studies demonstrated the nitrogen-retaining activity of synthetic testosterone in hypogonadal men.
Joseph Cofrancesco, M.D. is a fellow in general internal medicine at the Johns Hopkins University School of Medicine.














No comments:
Post a Comment